PULMONARY FIBROSIS
The term “Pulmonary” refers to lung while “Fibrosis” means scar tissue; similar to scars present on the skin due to old injuries or surgeries.
Thus, pulmonary fibrosis refers to lung scarring and eventual tissue scarring that would consequently hinder oxygen from entering the bloodstream. Ultimately, low oxygen levels (and the rigid scar tissue itself) lead to shortness of breath, particularly when walking or exercising.
POTENTIAL RISK FACTORS
PULMONARY FIBROSIS SYMPTOMS

Fatigue
Chest pain or tightness

Difficulty breathing during sleep (sleep apnea)

Chronic heartburn - acid reflux (GERD)

Shortness of breath with or without activity that worsens over time

Dry, hacking cough that lasts long time
Wet cough that produces mucus

Unexplained weight loss
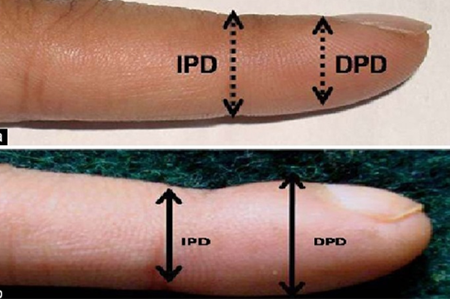
PULMONARY FIBROSIS PATIENT FINGERS (CLUBBING)
PULMONARY FIBROSIS DIAGNOSIS
PULMONARY FIBROSIS TREATMENT
The scarring of the lungs that occurs with idiopathic pulmonary fibrosis cannot be reversed. However, some treatments may improve symptoms temporarily or slow the progression of the disease:
1- Vaccination:
Influenza and Pneumococcal vaccine should be offered to patients with lung fibrosis, since such infections can adversely affect the quality of life in patients with interstitial lung disease.
2- Acid Reflux Related Life Style Modification:
- More studies emphasize the importance of controlling acid reflux to prevent disease progression and reduce exacerbation.
- Elevating the angle of bed slept on.
- Avoid foods known to cause reflux ; fatty foods, spicy foods, acidic foods, like tomatoes and citrus, mint, chocolate, onions, coffee or any caffeinated beverages, carbonated beverages.
- Eat smaller meal portions.
- Don’t lie down after eating: wait at least three hours before you lie down after a meal.
3- Oxygen Therapy:
Oxygen is usually administered through a pronged tube that is placed just under the nose. Oxygen therapy may be administered only during sleep or during exercise, but can also be administered for 24 hours as the disease progresses.
Oxygen therapy can help:
- Reduce shortness of breath.
- Improve exercise capacity.
- Possibly maintain patient ability in oreoareing for a lung transplant.
4- Pulmonary Rehabilitation:
A standard treatment for people with chronic lung disease. However, it does not replace medical therapy. It is used alongside medical treatments to help patients function to their best capabilities.
5- Medications:
There are currently two medications which have been proven to slow the progression of IPF. Your doctor can help you decide if one of these is right for you. In addition, if you have gastro-esophageal reflux, your doctor may prescribe other therapies to reduce the acid in your stomach, as this may slow the progression of IPF.
6- Exercise, with or without Oxygen:
Need support from family, friends and community.